Posterior Tibial Tendonitis and Dysfunction
Stride Footcare in West End, Brisbane, provides diagnosis and treatment for Posterior Tibial Tendon Dysfunction (PTTD). PTTD can lead to significant pain, instability, and mobility issues, but with early intervention and the right treatment plan, we can help you get back on your feet.
What is PTTD (Posterior Tibial Tendon Dysfunction)?
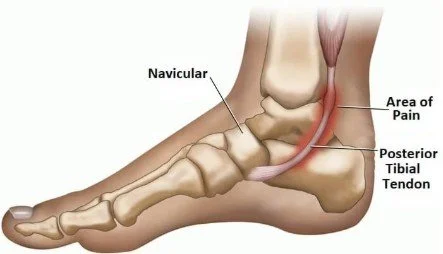
PTTD refers to the dysfunction or degeneration of the posterior tibial tendon, which plays a critical role in supporting the arch of your foot. This tendon helps to hold the foot’s arch in place and allows you to perform activities like walking, running, and standing.
When the tendon becomes weakened or damaged—either due to injury or overuse—it can cause pain, swelling, and a progressive flattening of the foot arch. If left untreated, PTTD can lead to flatfoot (collapsed arches) and cause long-term instability.
Symptoms of PTTD
The symptoms of Posterior Tibial Tendon Dysfunction can vary depending on the stage of the condition, but the most common include:
Pain and tenderness along the inside of the ankle
Swelling on the inner side of the ankle
Flattening of the foot arch
Heel pain or pain when walking on uneven surfaces
Difficulty standing on tiptoe on affected side
The feeling that your foot is rolling inward (foot collapse)
Pain that worsens with activity
If you experience any of these symptoms, it's important to see a podiatrist as early intervention can prevent the condition from progressing.
Risk Factors of PTTD
While anyone can develop PTTD, certain factors may increase your risk. These include:
Gender - PTTD is more common in women. Research suggests that the condition may be linked to the biomechanics of the female foot, along with hormonal changes, particularly in postmenopausal women.
Age - The risk of developing PTTD increases with age, typically affecting adults over the age of 40.
Overuse and Repetitive Strain - Activities that involve excessive running, walking, or standing for long periods can place strain on the posterior tibial tendon and increase your risk of developing PTTD.
Obesity - Excess body weight can place additional stress on the feet, contributing to tendon wear and degeneration.
Flat Feet - People with flexible flat feet or who have had flat feet from birth are at higher risk of developing PTTD.
Previous Ankle Injuries - Ankle sprains, fractures, or other injuries that affect the tendons and ligaments in the lower leg can lead to PTTD.
Treatment Options for PTTD
The treatment plan for PTTD will depend on the severity of the condition, but we offer a range of options designed to reduce pain, improve foot function, and prevent further tendon damage:
Custom Foot Orthotics
Custom foot orthotics help support the arch, reduce strain on the posterior tibial tendon, and improve your gait. Orthotics are particularly effective in the early stages of PTTD.
Stretching & Strengthening Exercises
A tailored exercise program to strengthen the posterior tibial tendon and surrounding muscles, as well as stretching exercises to improve flexibility, can help restore function and prevent the progression of the condition.
Bracing
If you have more advanced PTTD or need additional support, AFOs (Ankle-Foot Orthosis) can help provide stability to the foot and ankle, preventing further collapse of the arch. Braces such as the EXO-L or EXO-UP are used in cases where there’s significant tendon dysfunction or foot drop caused by nerve damage.
Physical Therapy
Working with a physical therapist can help improve mobility, strengthen muscles, and restore function in the affected foot and ankle.
Shockwave Therapy
For chronic tendon issues, we may recommend shockwave therapy, which uses high-energy sound waves to stimulate healing in the affected tissue.
Surgery
In severe cases where conservative treatments do not provide relief, surgery may be required to repair or reconstruct the posterior tibial tendon.
Preventing PTTD
While you may not be able to completely prevent PTTD, there are several steps you can take to reduce your risk:
Wear supportive shoes that offer good arch support and cushioning.
Strengthen your calves, ankle muscles and calves regularly
Stretch regularly to improve flexibility and reduce the risk of muscle and tendon injuries.